As millions of people are recovering from COVID-19, an unanswered question is the extent to which the virus can “hide out” in seemingly recovered individuals. If it does, could this explain some of the lingering symptoms of COVID-19 or pose a risk for transmission of infection to others even after recovery?
I am a physician-scientist of infectious diseases at the University of Virginia, where I care for patients with infections and conduct research on COVID-19. Here I will briefly review what is known today about chronic or persistent COVID-19.
What is a chronic or persistent viral infection?
A chronic or persistent infection continues for months or even years, during which time virus is being continually produced, albeit in many cases at low levels. Frequently these infections occur in a so-called immune privileged site.
What is an immune privileged site?
There are a few places in the body that are less accessible to the immune system and where it is difficult to eradicate all viral infections. These include the central nervous system, the testes and the eye. It is thought that the evolutionary advantage to having an immune privileged region is that it protects a site like the brain, for example, from being damaged by the inflammation that results when the immune system battles an infection.
An immune privileged site not only is difficult for the immune system to enter, it also limits proteins that increase inflammation. The reason is that while inflammation helps kill a pathogen, it can also damage an organ such as the eye, brain or testes. The result is an uneasy truce where inflammation is limited but infection continues to fester.
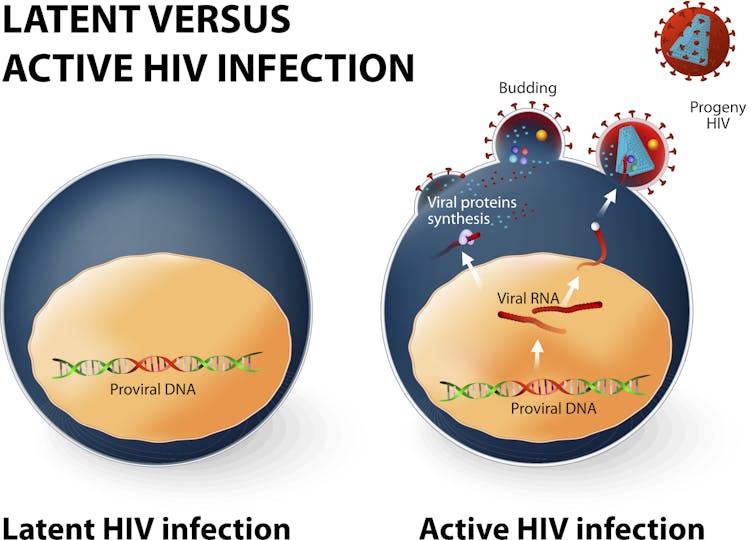
A latent infection versus a persistent viral infection
But there is another way that a virus can hide in the body and reemerge later.
A latent viral infection occurs when the virus is present within an infected cell but dormant and not multiplying. In a latent virus, the entire viral genome is present, and infectious virus can be produced if latency ends and the infections becomes active. The latent virus may integrate into the human genome – as does HIV, for example – or exist in the nucleus as a self-replicating piece of DNA called an episome.
A latent virus can reactivate and produce infectious viruses, and this can occur months to decades after the initial infection. Perhaps the best example of this is chickenpox, which although seemingly eradicated by the immune system can reactivate and cause herpes zoster decades later. Fortunately, chickenpox and zoster are now prevented by vaccination. To be infected with a virus capable of producing a latent infection is to be infected for the rest of your life.
How does a virus become a latent infection?
Herpes viruses are by far the most common viral infections that establish latency.
This is a large family of viruses whose genetic material, or genome, is encoded by DNA (and not RNA such as the new coronavirus). Herpes viruses include not only herpes simplex viruses 1 and 2 – which cause oral and genital herpes – but also chickenpox. Other herpes viruses, such as Epstein Barr virus, the cause of mononucleosis, and cytomegalovirus, which is a particular problem in immunodeficient individuals, can also emerge after latency.
Retroviruses are another common family of viruses that establish latency but by a different mechanism than the herpes viruses. Retroviruses such as HIV, which causes AIDS, can insert a copy of their genome into the human DNA that is part of the human genome. There the virus can exist in a latent state indefinitely in the infected human since the virus genome is copied every time DNA is replicated and a cell divides.
Viruses that establish latency in humans are difficult or impossible for the immune system to eradicate. That is because during latency there can be little or no viral protein production in the infected cell, making the infection invisible to the immune system. Fortunately coronaviruses do not establish a latent infection.

Could you catch SARS-CoV-2 from a male sexual partner who has recovered from COVID-19?
In one small study, the new coronavirus has been detected in semen in a quarter of patients during active infection and in a bit less than 10% of patients who apparently recovered. In this study, viral RNA was what was detected, and it is not yet known if this RNA was from still infectious or dead virus in the semen; and if alive whether the virus can be sexually transmitted. So many important questions remain unanswered.
Ebola is a very different virus from SARS-C0V-2 yet serves as an example of viral persistence in immune privileged sites. In some individuals, Ebola virus survives in immune privileged sites for months after resolution of the acute illness. Survivors of Ebola have been documented with persistent infections in the testes, eyes, placenta and central nervous system.
The WHO recommends for male Ebola survivors that semen be tested for virus every three months. They also suggest that couples abstain from sex for 12 months after recovery or until their semen tests negative for Ebola twice. As noted above, we need to learn more about persistent new coronavirus infections before similar recommendations can be considered.
Could persistent symptoms after COVID-19 be due to viral persistence?
Recovery from COVID-19 is delayed or incomplete in many individuals, with symptoms including cough, shortness of breath and fatigue. It seems unlikely that these constitutional symptoms are due to viral persistence as the symptoms are not coming from immune privileged sites.
Where else could the new coronavirus persist after recovery from COVID-19?
Other sites where coronavirus has been detected include the placenta, intestines, blood and of course the respiratory tract. In women who catch COVID-19 while pregnant, the placenta develops defects in the mother’s blood vessels supplying the placenta. However, the significance of this on fetal health is yet to be determined.
[Deep knowledge, daily. Sign up for The Conversation’s newsletter.]The new coronavirus can also infect the fetus via the placenta. Finally, the new coronavirus is also present in the blood and the nasal cavity and palate for up to a month or more after infection.
The mounting evidence suggests that SARS-CoV-2 can infect immune privileged sites and, from there, result in chronic persistent – but not latent – infections. It is too early to know the extent to which these persistent infections affect the health of an individual like the pregnant mother, for example, nor the extent to which they contribute to the spread of COVID-19.
Like many things in the pandemic, what is unknown today is known tomorrow, so stay tuned and be cautious so as not to catch the infection or, worse yet, spread it to someone else.
Artikel ini diambil dari theconversation.com dengan judul “Does coronavirus linger in the body? What we know about how viruses in general hang on in the brain and testicles”, https://theconversation.com/does-coronavirus-linger-in-the-body-what-we-know-about-how-viruses-in-general-hang-on-in-the-brain-and-testicles-142878
Penulis/Editor : Professor of Medicine, University of Virginia
Foto Cover : Are there places in the body where SARS-CoV-2 can hide from the immune system? fotograzia / Getty Images